The abscess of the psoas muscle is a condition rare and difficult to diagnose, with a generally non – specific clinical presentation and sometimes forgotten in daily practice, leading to delayed diagnosis.
Description
The psoas muscle, elongated and fusiform, has a retroperitoneal anatomical arrangement; originates from the lateral borders of the 12th rib and the lateral vertebral borders of T12, as well as those of all lumbar bodies (L1 – L5) to end up inserting into the lesser trochanter of the ipsilateral femur by forming a common tendon with the iliac muscle ; it is innervated by the roots of L2, L3 and L4 before the formation of the femoral nerve. Its activity determines the flexion and lateral rotation of the femur.
Because they share a location in the posterior abdominal wall as well as tendon function and insertion with the iliac muscle, these muscles are commonly referred to as the “iliac psoas muscle”, where the latter, with a wide and flattened appearance, arises from the anterior aspect of the iliac bone and its radiated fibers pass over the joint capsule and under the inguinal ligament, until reaching the point of insertion.
The first medical description of a psoas abscess was made by Abeille, in 1854, with eight patients who showed pyogenic abscesses; Later, Mynter did it, in 1881, under the name of “acute psoitis” with a case of unknown origin that he presented to the Buffalo Medical Club.
Causes
There are a series of predisposing factors associated with the appearance of the disease:
• Previous trauma: falls from a height.
• Distant septic foci: hematogenous spread.
• Iatrogenesis: acupuncture.
• Senectud.
• Anemia.
• Injecting drug users.
• Immunodeficiency associated with:
- Mellitus diabetes.
- Colonic neoplasm.
- Renal neoplasia.
- Chronic renal insufficiency.
- Chronic liver disease.
- Malnutrition.
- Alcoholism.
- Parasitism.
- Rheumatoid arthritis.
- Corticotherapy.
Diabetes tends to appear as the dominant and predisposing factor in up to 64% of cases, followed by colonic and renal neoplasms, debilitating chronic diseases such as chronic renal failure, and liver diseases of this nature.
Likewise, Crohn’s disease and hip arthritis and / or sacroiliitis are associated with these conditions and share the same common pathway: immunosuppression.
Previous trauma, specifically falls from a height, suggests the presence of an infected hematoma within the iliopsoas sheath. The presence of these factors ranges in 35-57.8% of the cases evaluated. There are also reports of exotic cases secondary to epidural obstetric anesthesia that lead to osteomyelitis, discitis, and psoas abscesses, as well as those that appear after performing cystostomies for acute urinary retention; For those in whom the existence of baseline immunodeficiency is not determined, it is proposed to rule out the existence of a secondary psoas abscess, according to the suggestion of some authors.
The microbiological evaluation identifies the following microorganisms, as the most frequently isolated according to various series:
• Staphylococcus aureus (18% – 90%) • Escherichia coli (9% – 21%) • Proteus mirabillis • Mycobacterium tuberculosis (36%) • Group B Streptococcus (9%) • Bacteroides fragilis • Pseudomonas aeruginosa • Prevotellasp. • Streptococcus mitisy • Brucellasp. • Salmonella enteritis (9%) • Polymicrobial flora (18 to 29.4% of the cultures, not related to any predisposing factor or concomitant process)
Symptoms
Generally, the clinical presentation is nonspecific, since there is no direct contact with the peritoneum by the inflamed area and the course of the same is usually prolonged with more frequent symptoms such as abdominal or lumbar pain (whose presentation varies between 76 – 91 %) and pain limiting flexion-extension of the homo-lateral hip or “psoas sign” (in 15-69%), where painless flexion of the thigh is found on the hip and pain is triggered when extending the lower limb .
Likewise, the presence of the classic triad: fever, abdominal-lumbar pain and limitation of hip movement, secondary to psoas spasm, appears in 35-87% of cases. Individually, fever can be identified, alone or associated with other signs, in 90-100% of cases.
Subacute or chronic presentation, in which symptoms persist for more than seven days, can be identified in 83% of patients. In other series, an evolution of symptoms was found even greater than 30 days in up to 64% of cases; a diagnostic delay is considered an average of six weeks.
Atypical presentations such as neuropraxia of the femoral nerve, or irritability of the prostate in association with hip pain, should alert the clinician to consider the entity.
The conclusion is that psoas abscess is a disease with nonspecific characteristics, which entails a delay in diagnosis and a non-negligible morbidity and mortality, whose clinical suspicion is based on the presence of the following signs and symptoms:
• Inguino-femoral or rarely lumbar pain irradiated or not to the lower limb. • Sign of the psoas present. • Antalgic lameness when dissecting the psoas sheath leading to severe flexion deformity of the hip. • Hard and painless mass on the iliac fossa, in 50% of chronic cases
Presentation varieties
The literature refers to two forms:
A. Typical: Presence of fever, lumbar pain or pain in the groin and front of the thigh.
B. Atypical: More insidious and consistent with fever and abdominal discomfort
Differential diagnosis Acute appendicitis : It usually offers the highest number of diagnostic errors; The presence of onset of periumbilical pain, nausea, vomiting, McBurney’s and / or Blumberg’s sign helps to differentiate it.
Septic arthritis of the hip : Absence of the psoas sign, painful hip mobility in all directions, positive hip puncture.
Sacro-iliac arthritis or iliac osteo-myelitis : Triad of pain over the sacro-iliac joint, pain on compression of the iliac crest distraction and pain on lateral elevation in abduction on the involved side.
Others : Rheumatic fever, discitis, soft tissue abscess, lymphoma, pelvic inflammatory disease, etc.
Complementary exams
Laboratory
The clinical picture is usually accompanied by leukocytosis with a left shift, anemia, and elevated erythrocyte sedimentation or erythrocyte sedimentation rate.
In some articles, urinary tract infection (UTI) (52%) with enteric microorganisms as etiological agents (Escherichia coli44% and Klebsiella spp. 24%) is reported as the most common etiological source. Other authors most frequently identified enteric anaerobic and gram-negative bacilli, followed by Staphylococcus aureus and Mycobacterium tuberculosis.
Imaging studies
Before having adequate imaging techniques, up to 70% of cases were diagnosed by necropsy.
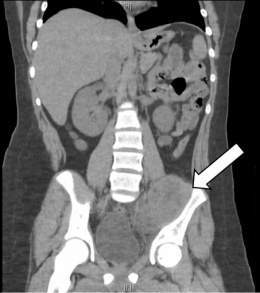
Currently, the diagnostic efficacy of ultrasound and computed tomography (CT) reaches 57% and 91% respectively, and the diagnosis can be established in selected cases by magnetic resonance imaging (MRI), although CT is the procedure of choice.
Plain X-ray of the abdomen In this study, the usefulness for diagnosis is very limited and only 33% of the films identify an increase or effacement of the psoas line on the affected side. One of its characteristics is that, to a certain extent, it allows the identification of bone lesions when chronic conditions are present, but it also requires adequate intestinal preparation.
Other identifiable radiographic findings include iliac fossa opacity, gas around the psoas, and antalgic scoliosis.
Ultrasound Currently, the most used technique in the initial evaluation of patients with suspected PA is abdominal ultrasound, which confirms the diagnosis in 40 – 57% of cases, revealing a liquid collection over the psoas area.
The disadvantages that are usually associated with this test are: • It cannot be performed adequately in obese patients. • Does not identify small abscesses and / or phlegmons. • Interposition of intestinal gas. • It is operator-dependent, which shows that it depends largely on the experience of the radiologist who performs it.
Contrast abdominal tomography (CT) This method confirms the diagnosis and defines the extent of the abscess; it is considered the imaging technique with the highest diagnostic value for the diagnosis of PA, with a sensitivity that varies between 80 and 100%. In the same way, it allows to guide joint punctures or the drainage of the abscess.
Scintigraphy The Ga 67 scintigraphy can facilitate early diagnosis; it is superior to CT in the concomitant demonstration of infectious foci in other sites, such as vertebral or iliac osteomyelitis, sacroiliac septic arthritis or the presence of multiple bone abscesses, although its use is infrequent in practice.
Magnetic resonance imaging (MRI) MRI is useful to assess the spread of infection to the epidural space and soft tissues; shows enhancement of the infected joint facet on the T1 image after gadolinium injection, as well as better soft tissue resolution and the ability to demonstrate the abscess walls without the need for other intravenous contrast media. Although this study surpasses all the others, its high cost and the general lack of availability in our setting limits its use.
Other studies The excretory urography and the colon by enema may show renal and / or urethral displacement, associated colic affection and / or displacement of the cecum or sigmoids. Endovenous pyelography was once considered the diagnostic method of choice, but it only guided the diagnosis in 50% of cases. The barium enema for Crohn’s disease can reveal the presence of a communicating fistula between the digestive tract and the abscess.
Treatment
Previously, antibiotic coverage accompanied by skin traction was proposed for early diagnosed cases, and surgery should be reserved for those patients in whom this management failed or when a diagnosis was made at an advanced stage of its evolution.
At present, adequate treatment is based on antibiotic therapy in addition to percutaneous drainage guided by CT or ultrasound; in certain cases surgical drainage is necessary.
In the light of current knowledge, it can be affirmed that percutaneous drainage directed by ultrasound or CT (ideally) becomes the first-line therapeutic choice compared to the open procedure, it also facilitates the rapid obtaining of samples for culture, it presents a low morbidity and ensures resolution of the abscess in 75-95% of cases. This is applicable to both primary and secondary abscesses, avoiding further intervention. Faced with treatment failure, open drainage should not be postponed and open surgery is also reserved for certain well-determined cases such as non-accessible collections, multi-loculated abscesses,patients who require surgery due to their underlying disease and the open approach is even proposed for all cases originating from Crohn’s disease or if gastrointestinal pathology is suspected.
The possibility of performing drainage with placement of a percutaneous catheter directed by CT or ultrasound is recognized, with which a success rate of up to 80% is achieved, requiring that the collection be well defined and organized.
Classically open drainage is performed by lumbotomy through an incision 3 cm from the iliac crest on the involved side, parallel to it and approximately 10 cm in length. Once the oblique and transverse muscles, as well as the transversalis fascia, have been disclosed, the extraperitoneal and posterior muscles are disclosed until the collection is identified and drained.
Another approach and drainage route is through the anterior aspect of the thigh ipsilateral to the collection, although some authors consider that when drainage is performed through this route or at the groin level, evacuation is inadequate and there are high failure rates.
The integrated medical-surgical treatment carries the antibiotic scheme for a variable period according to the etiology of the abscess and its clinical evolution; The intravenous administration of the antibiotic is maintained for the first three to four weeks and the oral administration is continued for fifteen days or one more month (six to eight weeks of total management). In an empirical and early way, the management begins looking for a coverage against gram positives (S. aureus), anaerobes and gram negative germs, until having an identification by means of the appropriate cultures. It is recommended to start empirical antibiotic therapy before drainage.
An inflammatory process inside the parotid gland, with or without the formation of an abscess , may be due to an obstruction of Stensen’s duct due to inflammation , esophageal foreign bodies , especially salivary stones, direct spread of an infection of neighboring structures, especially of the facial spaces of the neck , or as a complication of abdominal or pelvic operations .
