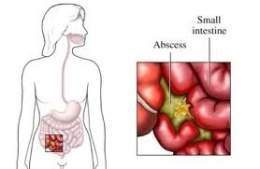
Abdominal abscess or intra- abdominal abscess are purulent collections formed in the peritoneal cavity and limited by adhesions of inflammatory cause between intestinal loops , mesentery , omentum , diaphragm and other abdominal viscera.
Causes
It can be caused by a ruptured appendix, ruptured intestinal diverticula, inflammatory bowel disease, a parasitic intestinal infection (Entamoeba histolytica), or another condition.
Risk factor’s
Risk factors include having a history of appendicitis , diverticulitis , perforated ulcer disease, or any surgery that may have infected the abdominal cavity.
Symptoms
- Abdominal pain and bloating.
- Shaking chills.
- Diarrhea .
- Fever .
- Lack of appetite
- Sickness.
- Rectal tenderness and fullness.
- Vomiting .
- Weakness.
Location
They can be found according to the different compartments of the abdomen such as:
- Supramesocolic space also called subphrenic, and ramesocolic space . The first is divided on the right side into the suprahepatic and infrahepatic space . The suprahepatic space is divided according to the relationship with the falciform ligament of the liver into right suprahepatic and left suprahepatic. The infrahepatic or subhepatic space is divided into 2 zones, which are delimited by the round and venous ligaments and later by the Winslow hiatus that communicates it with the lesser sac.
- The left area of the supramesocolic space is extensive, called the left suprahepatic space, splenic cell, or left subphrenic space. The inframesocolic space, delimited laterally by the colic framework, is divided by the mesentery into: the right mesenterycolic and the left mesenterycolic, larger and open towards the pelvic space.
- Lateral to the ascending and descending portions of the colon are the right and left parabolic or parietocolic gutters, frequent sites of purulent collection in septic abdominal processes.
- The pelvic space is a cul-de-sac that descends in the form of a rectovesical fold in men and rectouterine in women (Douglas cul-de-sac), which is accessible to digital exploration and puncture / drainage, both rectally and rectally. vaginal.
According to these anatomical divisions, the location of intra-abdominal abscesses is determined by the place of contamination; that is, by the point where the visceral perforation occurs ; by the anatomy of the intraperitoneal spaces and by the flow of exudates within the abdominal cavity .
Assessing the position that the patient tends to adopt on his sickbed: supine position , or Fowler or semi-sitting position, there will be 2 areas of fluid accumulation: subphrenic and pelvic space.
Given the rise of the pelvic fluid through the parietocolics towards the subphrenic space, the development of abscesses at a distance from the initial septic focus is not surprising. Furthermore, due to the obstacle posed by the phrenic ligament in the ascent of the exudates on the left side, it is to be assumed that right subphrenic abscesses are more frequent than left abscesses. Of course, this location occurs after gastric , colic or splenic surgeries . Purulent collections located in the lesser sac are infrequent, although they occur in posterior gastric wall perforations and in pancreatitis.
In correspondence with the frequency of location of intra-abdominal abscesses, different series classify it on the right side in 64% (right suprahepatic space), in 28% in the left and in both sides in 6%. Of the subphrenic abscesses, 90% are intraperitoneal, 6% extraperitoneal, and the rest combined.
According to its pathogenesis, the development and formation of an intra-abdominal abscess requires a series of conditions. The germs responsible for this septic process act not only by proliferating and invading the peritoneal space, but also through various mechanisms that contribute to creating the necessary conditions for this proliferation.
Faced with these mechanisms, the body opposes various defensive systems, destroying the bacterial inoculum or locating it to prevent its dissemination. The symptoms of intra-abdominal abscesses are varied and generally not very evident. It depends on the site of the septic focus, the previous treatment, the type of surgical procedure and the use or not of drains, antibiotics and drugs that reduce the inflammatory response.
Its clinical manifestation consists of a septic picture, with fever, tachycardia, sweating, weight loss, anorexia, leukocytosis and anemia. There may be pain in an area of the abdomen, which may be spontaneous or on palpation. The pain can sometimes be localized, other times vague, deep or diffuse and referred to the abdomen, thorax, rib margin or lumbar fossae. By neighborhood there may be pleural effusion, pulmonary atelectasis, diaphragmatic immobilization when it is subphrenic.
Signs and symptoms of a digestive nature can be found, such as subocclusive symptoms, rectal urgency, diarrhea or lower urinary symptoms when the purulent collection is pelvic in location.
Diagnosis
Given the few clinical manifestations, especially in the early stage, it is necessary to use diagnostic techniques to detect the abscess collection.
The X – ray with lateral and Posteroanterior, thoracic, abdominal and centered on the diaphragm, can provide signs indirect: elevation of the hemidiaphragm, loss of their contours and decreased mobility, pleural effusion and mass effect at the abdomen. Contrast X-rays of the gastrointestinal tract can confirm displacement or compression of organs or leak responsible for communication with the abscess. The scintigraphy is based on demonstrating an expansive lesion that occupies space in the liver, spleen or at the level of the mesentery.
The ultrasound (US) has marked progress in the location of intraabdominal abscesses, especially those location solid organs (liver, kidney, pancreas and spleen), perihepatic in flanks, and paracolic surface. The appearance offered by the US in the AIA is of rounded or oval collections of an expansive, irregular and confused nature due to the diffusion of the echoes due to the echogenicity of the content.
Regarding surgical ultrasonography, this avoids some drawbacks of the one performed through the skin, some such as the interposition of intestinal gas and fatty tissue and is very useful in helping surgeons in locating abscesses before the start of tissue dissection and search.
The [[Computerized axial tomography | computerized axial tomography]] (CT), is the method par excellence for the diagnosis of AIA, and its characteristics can be focused, in that it is precise, fast and effective, since it shows an anatomical image useful, eliminating the inconveniences of the US. This procedure can also be performed with contrast, both for the gastrointestinal tract and intravenously to opacify the urinary tract.
Obvious signs of localized intra-abdominal sepsis or a more or less diffuse collection, is the presence of air-fluid levels inside the septic accumulation or the existence of gaseous cavities. A useful sign is thickening of the aponeurotic plane in contact with the AIA.
The definitive diagnosis and treatment in intra-abdominal purulent collections or AIA will be based on puncture and percutaneous aspiration under the guidance of US or CT, study of the fluid or the intra-abdominal collection by culture with the demonstration of the etiologic agent. Open surgical treatment of an intra-abdominal abscess is not considered an initial remedy, but is carried out as long as it fails through puncture and the selective use of antibiotic therapy .
Exams
A complete blood count can show a white blood cell count that is above normal. A group of comprehensive metabolic tests can show liver , kidney, and blood chemistry problems .
A CT scan of the abdomen usually reveals an intra-abdominal abscess. After the scan is done, a needle may be placed through the skin into the abscess cavity to confirm your diagnosis and treat it.
Other tests may include:
- Abdominal X-ray.
- Ultrasound of the abdomen.
- Sometimes a surgery called a laparotomy may be needed to diagnose the condition.
Treatment
It requires intravenous antibiotic therapy and drainage. Drainage involves inserting a needle through the skin into the abscess, usually with X-ray guidance. The drainage tube is left in place for days or weeks until the abscess clears.
Sometimes abscesses cannot be safely drained in this way. In such cases, surgery should be performed under general anesthesia (the patient is unconscious and painless). An incision is made in the belly (abdomen), and then the abscess is drained and cleaned. The drainage tube is left in the abscess cavity and remains there until the infection clears.
Complications
- Reappearance of the abscess.
- Rupture of an abscess.
- Spread of infection into the bloodstream.
- Generalized infection in the abdomen.
