Elastic artery by virtue of the movements of the knee joint (continuous flexion and extension). By changing its structure and losing elasticity, it does not support these movements and thromboses.
Popliteal hollow
In human anatomy, the popliteal fossa is a more or less rhomboidal depression with a vertical major axis, located in the region of the animal legs, which can be seen in the posterior part of the knee, especially when the leg is flexed or semi-flexed.
The popliteal fossa is limited by six walls, mainly muscular and aponeurotic:
- Superolateral wall: the crural biceps muscle.
- Super-internal wall: the semimembranosus, semitendinosus, internal rectus and sartorius muscles.
- Inferoexternal wall: the external twin.
- Inferno-internal wall: the internal twin.
- Anterior wall: the femur and the popliteal muscle .
- Posterior wall: the aponeurosis of the popliteal region, and integuments.
Structure
From the outside in, the greater sciatic nerve is located at the level of the superior angle of the popliteal fossa, it bifurcates in its terminal branches: the internal popliteal sciatic nerve or tibial nerve and the external popliteal sciatic nerve or common peroneal nerve.
The popliteal vein occupies the median plane, between the artery and the nerve of the region. At the level of the joint line it receives the external saphenous vein; the latter runs along the floor of the popliteal fossa, and before emptying into the popliteal vein it crosses to the internal side of the internal popliteal sciatic nerve.
In the deepest plane is the popliteal artery (it should be noted that it becomes the popliteal artery when it crosses the ring of the third adductor or femoral hiatus , highlighting that previously, it was called the femoral artery), resting on the skeleton, it descends obliquely outwards, until it reaches the soleus ring, here it ends up dividing, in the tibiofibular trunk and in the anterior tibial artery . The popliteal hollow corresponds to the hamstring, in common language.
Popliteal artery entrapment syndrome
Anatomical state
The popliteal artery is the continuation of the femoral artery. It owes its name to the deep position it occupies on the posterior aspect of the knee joint, at the bottom of the popliteal fossa. It is the trunk of origin of the feeding arteries of the leg and foot.
The popliteal artery begins on the medial border of the femur, at the third adductor ring, about 8 cm above the joint line of the knee. It ends at the soleus ring, where it bifurcates into its two terminal branches, the anterior tibial artery and the tibiofibular trunk. Its average length varies between 17 and 18 cm.
On its way out of the Hunter’s duct, the artery descends through its upper part or first portion, obliquely, outwards. Then it bends and becomes vertical, descending along the axis of the popliteal rhombus. This is your second portion, which is not axial, but is located somewhat within the midline.
Starting from the tibial plateau, it is called the third portion and follows the same path as its anterior segment. These three divisions of the popliteal artery are practical from the anatomical point of view in vascular surgery. It is closely related to the popliteal vein and the internal popliteal sciatic nerve. The popliteal is one of the most mobile arteries in the body (extension and flexion of the knee forces the artery to bend frequently).
Etiology
When the lesions are of the atherosclerotic type, they are due to conditions that also affect the superficial femoral artery, which is why the previous article called it “Femoropopliteal obliteration”. Usually in these cases, Hunter’s duct occlusion with distal progression occurs. Popliteal arteriosclerosis, in its most distal form, is usually more severe because collateral circulation is less likely to develop in this area.
Special circumstances that can cause ischemia
Primary popliteal artery thrombosis
In certain circumstances, the popliteal artery loses its mobility and reacts to repeated trauma (its own pulsatility) with occlusion. This primary popliteal artery thrombosis was described by Boyd and closely resembles Hunter’s duct arteriopathy described with Palma.
Clinically it occurs in young people, under 35 years of age. The most striking symptom, and nothing short of exclusive, is intermittent claudication in the calf. The disease is always local. There are never general signs of thromboangiitis or arteriosclerosis. The pathological anatomy shows the absence of inflammatory or degenerative changes in the arterial wall.
The clinical suspicion can be confirmed by Doppler and ipsilateral percutaneous femoral puncture arteriography reveals a short segmental occlusion of the popliteal in its second / third portion. Resection of the obliterated sector and vein graft is the most recommended therapy.
Thrombosis of a popliteal aneurysm
The popliteal artery is, in order of frequency, the second place, after the aorta, where aneurysms of arteriosclerotic etiology are located. Most often they are bilateral (50%). They have a predilection for males and generally occur in people over 50 years of age.
If not treated surgically, popliteal aneurysms have serious complications: embolism, thrombosis, ruptures, etc. The tendency to embolism and / or thrombosis is due to the presence within the aneurysmal sac of the mud, made up of old clots that completely fill the cavity, in such a way that a popliteal that does not appear dilated is frequently seen on arteriography.
Thus, there is a disagreement between computed tomography (CT) or magnetic resonance imaging (MRI) and arteriography. This thrombotic tendency of the popliteal aneurysm is greater than that of other aneurysms, which results in ischemia, which can be severe due to the scarcity of collaterals in this arterial path (Fig. 1).
Symptoms are characterized by the presence of a pulsatile lump that is usually discovered by the patient himself by chance. Given the deep location in a bony hole of the popliteal artery, these aneurysms remain asymptomatic for a long time.
Diagnosis is easy upon palpation of a slightly transverse, pulsatile, expandable tumor that can be partially reduced. Echo-Doppler, CT and / or MRI corroborate the diagnosis .
Arteriography considerably facilitates the practice of surgical resection and interposition of a saphenous vein or PTFE graft.
Spontaneous intraaneurysmal thrombosis is a complication that can lead to healing of these aneurysms, with disappearance of compression discomfort, or it can lead to an ischemic picture, which can be acute with serious repercussions for the limb, or chronic, with symptoms of intermittent claudication of the twin mass.
It is possible in some patient that the formation of the aneurysm and its spontaneous thrombosis go unnoticed, discovering the tumor accidentally when exploring the patient, in which case, a differential diagnosis will be made with the other possible tumors of the knee: sarcomas, hemarthrosis, cyst of Becker, etc.
Cystic degeneration of the popliteal artery
Hiertong, Lindberg and Rob described, in 1957 , 4 cases of segmental obliteration of the popliteal artery due to cystic degeneration of the adventitia. All the patients were young, with no previous history of trauma, with symptoms of intermittent claudication in the calf with a sudden onset. They did not present symptoms or signs of general vascular disease (arteriosclerosis, thromboangiitis).
The etiology is unknown, although it is assumed that the degeneration occurs by the same mechanism as the primary thrombosis described by Boyd. The lesion is located in the second portion of the popliteal, which is located above and below the obliteration of caliber and normal characteristics (first and third portions).
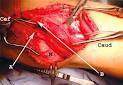
The mucosal degeneration is located outside the tunica media and inside the adventitia, leaving the arterial lumen occluded by the gelatinous mass under great tension. The walls of the cyst are lined by flat cells. Treatment is surgical and consists of removal of the affected arterial segment and interposition of a venous or PTFE graft (Figs. 2a and b).
Popliteal artery entrapment syndrome
The syndrome of entrapment of the popliteal artery is due to an external compression of the same, caused by the congenital anomaly in the development of the circulation of the popliteal fossa and / or of the musculature, preferably of the internal gastrocnemic muscle.
It was an Edinburgh medical student , Stuart, who first described the anatomical abnormality of the popliteal artery in relation to the medial calf muscle in 1879 when dissecting the amputated lower limb from a 64-year-old patient.
In 1959 , the Dutch Hamming made a definition of the picture and made the first surgical correction. In 1965 , Love and Whelan coined the term “popliteal artery entrapment syndrome” which is subsequently accepted worldwide.
There are several theories that can explain this anomaly. The vascular theory emphasizes the absence of development of the circulation of the popliteal fossa, maintaining the fetal situation posterior to the medial calf muscle. The muscular theory described by Carter and Eban highlights the persistence of the peroneal insertion of the medial gastrocnemius muscle, in an abnormal position, migrating to the supracondylar area of the femur. The mixture of both could explain the multiple possibilities that are observed in the type of compression of the popliteal artery.
Its incidence in the context of possible lesions of the popliteal artery is around 1%. However, a higher frequency is accepted, because the lesion can go unnoticed when the popliteal artery is occluded, which is why it is erroneously classified as arteriosclerotic disease in certain cases.
On the other hand, because it usually occurs in young people with slightly disabling symptoms, in some cases a correct diagnosis is not made. In fact, in general, these are men under 30 years of age, in a large number athletes and in whom between 25 and 30% of cases the condition is bilateral.
Its characteristic symptomatology is intermittent twin claudication. Given the suspicion of the lesion by clinical examination, a Doppler study should be carried out, which generally confirms a segmental occlusion of the popliteal artery. If the hemodynamic examination is normal, dorsiflexion tests of the foot with knee extension are performed, which will show the disease, with loss of the Doppler velocimetric wave.
Likewise, the technique of CT, MRI and / or ipsilateral percutaneous femoral puncture arteriography can be used, if possible the latter, with dorsiflexion of the foot, which is the position that will show an occlusion in the second / third portion of the popliteal artery.
In 1971 Delany and González made a classification into four types (figs. 3 ad).
I. The popliteal artery is situated medial and posterior to the medial calf tendon, which occupies a normal position.
II. The internal twin insertion is more lateral than normal and the popliteal artery passes under it.
III. An accessory bundle of the medial twin arises from the femur, more lateral than the main tendon, which is in a normal position. The popliteal artery is compressed by this accessory bundle.
IV. The popliteal artery is usually in its normal position but is compressed by a deep popliteal muscle inserted higher than normal or by a fibrous band.
The proposed therapy is surgical, and consists of the arterial release when it is permeable, if the artery is obliterated, the possibility of practicing a graft with saphenous vein or PTFE must be considered.
Sitology
Complete segmental occlusion of the popliteal artery manifests as intermittent claudication in the calf. In general, if it is a primary thrombosis, a cystic degeneration or a syndrome of the entrapment of the popliteal artery, the obliterations tend to park, in contrast to arteriosclerotic or arteritic lesions.
In the case of thrombosis of a popliteal aneurysm, the symptoms may be broader, since by compression of structures that accompany the artery (neuralgia, distal-popliteal venous thrombosis), either the symptoms of an ischemic picture due to embolization / thrombosis of the distal arterial axis (tibiofibular trunks), favored by emigration or mobilization of the thrombus that occupies the aneurysmal cavity.
Diagnosis
Differential diagnosis
Segmental obliteration of the popliteal produces symptoms of intermittent claudication in the calf, identical to that of femoropopliteal occlusion, so the same differential diagnosis should be considered here with all pain affecting the leg.
In the case of a thrombosed aneurysm of the popliteal artery, since there may be swelling of the knee or compression of the satellite structures, it is necessary to differentiate these pains that are located in the knee area.
Treatment
In case of chronic grade II ischemia not incapacitating for the patient, medical treatment can be followed. In cases III or IV, a saphenous vein graft or PTFE should be performed.
