They are a form of glioma with star-shaped cells . Often and for long periods they grow very slowly or not at all. Therefore, close observation rather than treatment is possible in some cases (especially those associated with neurofibromatosis ).
Symptoms
The general symptoms of an astrocytoma are the result of pressure growing in the skull . These symptoms are sore head , vomiting and changes in mental states. Other symptoms, such as drowsiness , lethargy, stubbornness, personality changes, conduct disorders, and problems with your mental faculties, occur early in one in four patients with malignant brain tumors.
In young children, the increasing pressure of an astrocytoma within the skull can elongate the head. Changes (such as swelling) can be seen at the back of the eye, where the blind spot is located. There are usually no changes in temperature, blood pressure, pulse, or respiratory rate except before death. Attacks with meningiomas, slow-growing astrocytomas, and oligodendrogliomas are more common than malignant gliomas.
Symptoms of astrocytomas vary depending on which part of the brain is located and is being affected by the tumor (or which gland or nerve). Sometimes the nature of the seizures can determine the location of the brain tumor .
Diagnosis
A neurological evaluation should be performed if the patient has increasing signs of mental dysfunction, new attacks, persistent headaches, or there is evidence of pressure within the skull such as vomiting or swelling or a bulge in the blind spot at the back of the eye.
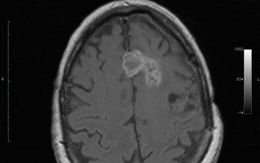
A neurologist (who is a doctor who has received special and additional training in the diagnosis and treatment of disorders of the brain, spinal cord, and nerves) performs a comprehensive examination, which may include an MRI scan, CT scan computerized (CT or CAT) scan or an X-ray of the chest to determine if the tumor has spread from some other part of the body.
An MRI usually finds low-grade astrocytomas earlier than a CT scan. A cerebral angiogram is very rarely used to diagnose a brain tumor, but it can be done before surgery .
Depending on the symptoms that the patient presents, specialized tests will be carried out. These tests include visual field, visual acuity, and hearing.
If the results of other tests are inconclusive, an examination of the fluid that surrounds the brain and spinal cord may be done. This is usually necessary.
Treatment
Treatment for a brain tumor depends on the nature of the tumor, how fast it is growing, the symptoms it causes, and where it is located. Various approaches are commonly used for its treatment. The surgery is usually done to provide a diagnosis and to improve symptoms. This should be enough to cure benign brain tumors.
Radiation therapy is required to treat gliomas. Radiation therapy may be beneficial for tumors that are short-lived and have spread from other parts of the body. Chemotherapy also benefits some patients with such brain tumors .
Childhood astrocytomas
It is a disease in which benign (not cancer) or malignant (cancer) cells form in the tissues of the brain. The cause of most childhood brain tumors is unknown. The signs and symptoms of astrocytomas are not the same in all children.
To detect (find) and diagnose childhood astrocytomas, tests that examine the brain and spinal cord are used .
Childhood astrocytomas are often diagnosed and removed by surgery.
- Certain factors affect prognosis (chance of recovery) and treatment options.
Parts of the central nervous system where they are most frequent
- Cerebrum : is the largest part of the brain at the top of the head. The cerebrum controls thinking, learning, problem solving, speech, emotions, reading, writing, and voluntary movement.
- Cerebellum : It is in the lower and posterior region of the brain (near the middle of the back of the head). The cerebellum controls movement, balance, and posture.
- Brainstem : is the part that connects the brain with the spinal cord. It is in the lowest part of the brain (just above the back of the neck). The brainstem controls breathing, heart rate, and the nerves and muscles used to see, hear, walk, speak, and eat.
- Hypothalamus : It is the area that is in the middle of the base of the brain and controls body temperature, hunger and thirst.
- Visual pathway : group of nerves that connect the eye to the brain.
- Spinal cord : A column of nerve tissue that runs from the brain stem down the center of the back. It is covered by three thin layers of tissue called membranes. The spinal cord and membranes are surrounded by vertebrae (back bones). The nerves in the spinal cord carry messages sent between the brain and the rest of the body, such as a message from the brain to move muscles or a message from the skin to the brain to perceive touch.
Signs and symptoms in children
The signs and symptoms depend on the following:
- Whether the tumor forms in the brain or spinal cord.
- Tumor size.
- How fast the tumor grows.
- Age and stage of development of the child.
Some tumors do not cause signs or symptoms. Childhood astrocytomas or other conditions can cause signs or symptoms. Check with your child’s doctor if he has any of the following:
- Headache in the morning or headache that goes away after vomiting.
- Nausea and vomiting
- Trouble seeing, hearing, and speaking
- Loss of balance and trouble walking.
- Worsening of writing or slow speech.
- Weakness or change in feeling on one side of the body.
- Unusual drowsiness
- More or less energy than usual.
- Changes in personality or behavior.
- Convulsive seizures .
- Weight loss or gain for no known reason.
- Increased head size (in infants).
Diagnosis
To detect (find) and diagnose childhood astrocytomas, tests that examine the brain and spinal cord are used. The following tests and procedures can be used:
- Physical exam and history : An exam of the body to check general signs of health, such as checking for signs of disease, such as lumps or anything else that seems abnormal. The history of the patient’s health habits is also recorded, as well as the medical history of their previous illnesses and treatments.
- Neurological exam : A series of questions and tests to check the brain, spinal cord, and nerve function. The test checks the person’s mental state, coordination, and ability to walk normally, as well as the functioning of the muscles, senses, and reflexes.
- Visual field exam: An exam to check a person’s visual field (the total area in which objects can be seen). With this test, central vision (how much a person can see when looking straight ahead) and peripheral vision (how much a person can see in all other directions when looking straight ahead) are measured. The eyes are examined one by one and the eye that is not being examined is covered.
- Gadolinium MRI (Magnetic Resonance Imaging): A procedure that uses a magnet, radio waves, and a computer to create a series of detailed images of areas inside the brain and spinal cord. A substance called gadolinium is injected into a vein. It collects around cancer cells and makes them appear brighter in the picture. This procedure is also called nuclear magnetic resonance imaging (MRI). Sometimes a spectroscopic magnetic resonance imaging (MRI) test is done during the same MRI test to look at the chemical composition of brain tissue.
Childhood astrocytomas are often diagnosed and removed by surgery. If doctors think there may be an astrocytoma, a biopsy may be done to remove a tissue sample. For tumors in the brain, a part of the skull is removed and a needle is used to remove a sample of tissue. Sometimes the needle is guided by a computer.
A pathologist looks at the sample under a microscope to check for cancer cells. If cancer cells are found, the doctor can safely remove as much of the tumor as possible during the same surgery. Because it can be difficult to tell the difference between different types of brain tumors, it is preferable that the child’s tissue sample be viewed by a pathologist experienced in diagnosing brain tumors.
The following test may be done on the tissue sample that was removed:
- Immunohistochemistry : A test that uses antibodies to identify certain antigens in a tissue sample. The antibody is usually attached to a radioactive substance or a dye that makes the tissue light up under the microscope. This type of study is used to determine the difference between different types of cancer. An MIB-1 test is a type of immunohistochemistry used to check whether the tumor tissue has an antigen called MIB-1. This allows you to see how quickly the tumor is growing.
Sometimes tumors form in a place that is difficult to remove. If the removal of the tumor causes physical, emotional, or cognitive problems, a biopsy is performed and further treatment is given afterwards. Children with NF1 may not need a biopsy or surgery to remove the tumor. Certain factors affect prognosis (chance of recovery) and treatment options. The prognosis (probability of recovery) depends on the following:
- Whether the astrocytoma formed in the CNS and whether it has spread.
- If cancer cells are left after surgery.
- The type and grade of the astrocytoma.
- If the child has NF1.
- If there are certain changes in the genes.
- Age of the child.
- Whether the astrocytoma has just been diagnosed or has recurred (come back).
For recurrent astrocytoma, prognosis and treatment depend on the time elapsed between the end of therapy and the time of recurrence.
Stages of childhood astrocytomas
Important points
- To plan cancer treatment, the grade of the tumor is used.
o Low-grade astrocytomas o High-grade astrocytomas
- After surgery, MRI images are taken.
To plan cancer treatment, the grade of the tumor is used.
The staging is the process used to determine the amount of cancer present and whether the cancer has spread. It is important to know the stage of the disease in order to plan treatment. There is no standard staging system for childhood astrocytoma. Treatment is based on the following aspects:
- Tumor grade.
• Whether the tumor was newly diagnosed or recurred (came back after treatment). The grade of the tumor tells how abnormal the cancer cells look under a microscope and how quickly the tumor is likely to grow and spread. The following grades are used:
Low-grade astrocytomas
Low-grade astrocytomas are slow-growing astrocytomas that do not spread frequently to other parts of the brain and spinal cord, or to other parts of the body. Low-grade astrocytomas can be:
- Grade I tumors (pilocytic tumors, which form like a cyst and look like normal cells)
- Grade II tumors (fibrillar cell tumors with a long or fibrous appearance).
There are many types of low-grade astrocytomas. This summary covers several types of low-grade astrocytomas:
- A glioma of the visual pathway is a type of low-grade astrocytoma that forms along the optic nerve pathway.
- A subependymal giant cell astrocytoma is a type of low-grade astrocytoma that can occur in children with tuberous sclerosis .
Children with type 1 neurofibromatosis may have more than one low-grade brain tumor
High-grade astrocytomas
High-grade astrocytomas are fast-growing and often spread to the brain and spinal cord . High-grade astrocytomas can be:
- Grade III tumors (anaplastic or malignant tumors).
- Grade IV tumors (glioblastomas, which spread the fastest).
In general, childhood astrocytomas do not spread to other parts of the body. After surgery, MRI images are taken. A magnetic resonance imaging (MRI) test is done a few days after surgery to determine how much tumor, if any, is left after surgery and to plan further treatment.
Recurrent childhood astrocytomas
A recurrent childhood astrocytoma is an astrocytoma that has recurred (come back) after it has been treated. The cancer may return to the same place as the first tumor or to other parts of the body. High-grade astrocytomas often recur within three years. Treatment Option Overview Important Points
- There are different types of treatment for childhood astrocytoma patients.
- Treatment of children with astrocytomas should be planned by a team of health care providers experienced in treating brain tumors.
- Some childhood brain tumors can cause signs or symptoms that begin before diagnosis and continue for months or years.
- Some cancer treatments can cause side effects months or years after treatment ends.
- Six types of treatment are used:
o Surgery o Observation o Radiation therapy o Chemotherapy o High-dose chemotherapy with stem cell transplant o Targeted therapy
- New types of treatment are being tested in clinical trials.
o Other drug therapy
- If fluid builds up around the brain and spinal cord, a bypass procedure may be done.
- Patients should consider participating in a clinical trial.
- Patients can join clinical trials before, during, or after starting their cancer treatment.
- It may take up testing.
Types of treatment for childhood astrocytoma patients
There are different types of treatment available for children with astrocytomas. Some treatments are standard (the treatment currently in use), and some are being tested in clinical trials. A treatment clinical trial is a research study that seeks to improve current treatments or obtain information on new treatments for cancer patients. When clinical trials show that a new treatment is better than the standard treatment, the new treatment may become the standard treatment.
Because cancer in children is rare, participation in a clinical trial should be considered. Some clinical trials are open only to patients who have not started treatment. Treatment of children with astrocytomas should be planned by a team of health care providers experienced in treating brain tumors.
Your child’s treatment will be overseen by a pediatric oncologist , who is a doctor who specializes in treating children with cancer. The pediatric oncologist works with other health care providers who are experts in treating children with brain tumors and who specialize in certain areas of medicine. These specialists can be the following:
- Pediatrician .
- Pediatric neurosurgeon .
- Neurologist .
- Neuropathologist .
- Neuroradiologist .
- Rehabilitation specialist .
- Radiation therapy oncologist .
- Endocrinologist .
- Psychologist .
Some childhood brain tumors can cause signs or symptoms that begin before diagnosis and continue for months or years.
Signs or symptoms caused by the tumor may begin before diagnosis and continue for months or years. It is important to talk with your child’s doctor about signs or symptoms caused by the tumor that may continue after treatment. Some cancer treatments can cause side effects months or years after treatment ends. Side effects that start during or after treatment and continue for months or years are called late effects. Late effects of cancer treatment may include the following conditions:
- Physical problems
- Changes in mood, feelings, thoughts, learning, or memory.
- Second cancers (new types of cancer)
Six types of treatment:
Surgery
Surgery is used to diagnose and treat childhood astrocytoma, as outlined in the General Information section of this summary. If cancer cells remain after surgery, further treatment depends on the following:
- Place where the cells that were left are.
- Tumor grade.
- Age of the child.
Even if the doctor removes all the cancer that is seen at the time of surgery, some patients are given chemotherapy or radiation therapy after surgery to kill any cancer cells that are left. Treatment given after surgery to lower the risk of the cancer coming back is called adjuvant therapy .
Observation
Observation consists of closely monitoring a patient’s condition without giving treatment until signs or symptoms appear or change. Observation is often used in patients with type 1 neurofibromatosis or a tumor that is not growing or spreading.
Radiotherapy
Radiation therapy is a cancer treatment that uses high-energy x-rays or other types of radiation to kill cancer cells or stop them from growing. There are two types of radiation therapy:
- External radiation therapy uses a machine outside the body to deliver radiation toward the cancer.
- Internal radiation therapy uses a radioactive substance sealed in needles, seeds, wires, or catheters that is placed directly in or near the tumor.
External radiation therapy is used to treat astrocytoma in children. The way it is given depends on the type of tumor and where it formed in the brain or spinal cord. Radiation therapy to the brain can affect growth and development in young children. There are certain forms of radiation therapy that can decrease damage to healthy brain tissue:
- For conformal radiation therapy, a computer is used to create a three-dimensional (3-D) image of the tumor and tailors the radiation beams to the shape of the tumor. This allows a higher dose of radiation to reach the tumor and causes less damage to the normal tissue around the tumor.
- Intensity modulated radiation therapy (IMR) uses computer-created images that show the size and shape of the tumor. Thin beams of radiation of different strengths are pointed at the tumor from different angles.
- Stereotactic radiation therapy uses a rigid frame head fitted to the skull to direct radiation directly at the tumor, causing less damage to the healthy tissue around it. The total radiation dose is divided into several smaller doses that are given over several days. This procedure is also called external-beam stereotactic radiation therapy and stereotaxic radiation therapy.
- Proton beam radiation therapy is a type of external radiation therapy that uses currents of protons (small, positively charged particles of matter) to kill tumor cells.
For children younger than 3 years old, chemotherapy may be given to delay or reduce the need for radiation therapy.
Chemotherapy
Chemotherapy is a cancer treatment that uses drugs to stop the growth of cancer cells, either by killing them or by preventing them from multiplying. When chemotherapy is taken by mouth or injected into a vein or muscle, the drugs enter the bloodstream and can reach cancer cells throughout the body ( systemic chemotherapy ). When chemotherapy is placed directly into the cerebrospinal fluid , an organ, or a body cavity such as the abdomen, the drugs mainly affect cancer cells in those areas ( regional chemotherapy ). For combination chemotherapymore than one anticancer drug is used. Systemic chemotherapy is used to treat children with astrocytomas. The way chemotherapy is given depends on the type of tumor and where it forms in the brain or spinal cord.
High-dose chemotherapy with stem cell transplantation
High-dose chemotherapy with stem cell transplantation is a way to give high doses of chemotherapy and replace blood-generating cells destroyed by cancer treatment. Stem cells (immature blood cells) are taken from the blood or bone marrow of the patient or a donor, and frozen and stored. After completion of chemotherapy, the stored stem cells are thawed and reinjected into the patient via infusion. These reinjected stem cells become the body’s blood cells and restore the body’s blood cells.
For a high-grade astrocytoma that comes back after treatment, high-dose chemotherapy with stem cell transplantation is used if there is only a small amount of tumor.
Targeted therapy
Targeted therapy is a type of treatment that uses drugs or other substances to identify and attack specific cancer cells without harming normal cells. There are different types of targeted therapy:
- Kinase inhibitors prevent cell multiplication and can prevent the growth of new blood vessels that tumors need to grow. Everolimus and sirolimus are kinase inhibitors used to treat subependymal giant cell astrocytomas.
- For monoclonal antibody therapy, antibodies made in the laboratory, from a single type of immune system cell, are used to stop cancer cells. These antibodies can identify substances on cancer cells or normal substances that can help these cells grow. Antibodies stick to these substances and kill cancer cells, block their growth, or prevent them from spreading. Monoclonal antibodies are given by infusion into a vein. They can be used alone or to deliver drugs, toxins, or radioactive material directly to cancer cells. Bevacizumab is a type of monoclonal antibody used to treat childhood astrocytomas.
- The inhibitors of protein kinase prevent the action of the proteins necessary for cell growth and can kill cancer cells. Vemurafenib is a BRAF kinase inhibitor used to treat recurrent high-grade childhood astrocytoma. Selmetinib and dabrafenib are types of protein kinase inhibitors that are being studied in the treatment of childhood astrocytomas.
Other drug therapy
The Lenalidomide is a type of angiogenesis inhibitor which prevents the growth of new blood vessels that a tumor needs to grow. If fluid builds up around the brain and spinal cord, a bypass procedure may be done. The derivation of the cerebrospinal fluid is a method used to drain fluid that accumulates around the brain and spinal cord . A cannula (long, thin tube) is placed into a ventricle (fluid-filled space) in the brain and inserted under the skin into another part of the body, often the abdomen. The cannula carries excess fluid from the brain to be absorbed elsewhere in the body.
